Recurrent thyroid cancer is a difficult topic to discuss. It is an emotional issue for the patient and an area of controversy for the endocrine surgeon.
First we need to clarify some terms and organize our discussion. Recurrent thyroid cancer is really persistent cancer. As we discussed earlier, thyroid cancer is generally indolent. It commonly progresses slowly and may be clinically inconspicuous for years. Frequently, total thyroidectomy is curative, but 40% or more of patients with papillary thyroid cancer may have metastatic disease in local lymph nodes. Mysteriously, less than 10% of these patients will develop clinically relevant recurrent disease. However, those that do have a significantly elevated risk of death from their recurrence. Even with no detectable lymph node disease, certain demographic, histologic and operative findings may predict more aggressive cancers that have a higher risk of recurrence.
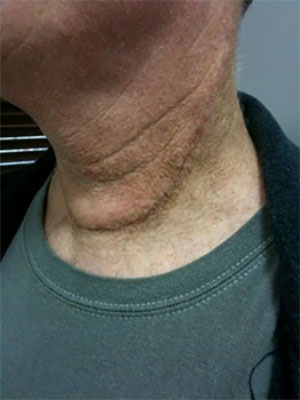
Our goal with surgery for recurrent thyroid cancer is to remove all malignant disease including malignant or potentially malignant lymph nodes. Patients older than 45, with tumors larger than 1.5 cm, with local invasion, lymph node metastases,or unfavorable histology are considered high risk for recurrence. These patients are usually given radioactive iodine (RAI) to destroy any microscopic tumor cells that may remain. Patients are then placed on a suppressive dose of thyroid medication. With this approach the majority of patients have their disease controlled. However, up to 30% of high risk patients and 10% of low risk patient may develop a clinical recurrence at some point in their life. This may manifest itself within months or may be delayed for many years. Therefore, life long followup is needed. Generally, we believe the earlier recurrent disease is detected the more effective it’s treatment.
On the next few pages we’ll discuss monitoring of patients and diagnosis of recurrence and treatment.
